Keep yourself and others safe: Do it all!
Protect yourself and those around you:
- Get vaccinated as soon as it’s your turn and follow local guidance on vaccination.
- Keep physical distance of at least 1 metre from others, even if they don’t appear to be sick. Avoid crowds and close contact.
- Wear a properly fitted mask when physical distancing is not possible and in poorly ventilated settings.
- Clean your hands frequently with alcohol-based hand rub or soap and water.
- Cover your mouth and nose with a bent elbow or tissue when you cough or sneeze. Dispose of used tissues immediately and clean hands regularly.
- If you develop symptoms or test positive for COVID-19, self-isolate until you recover.
For more information visit World Health Organizations coronavirus disease (COVID-19) page.
I am blown away by this COVID vaccine video, one of the coolest things I have seen in a long time pic.twitter.com/yREIETqtWh
— Sam (@SamIAm2021MD) November 12, 2021
COVID-19 mRNA vaccines deliver directions to make a protein that educates our immune system, so it will neutralize the virus in future encounters. The mRNA-containing lipid particles are taken up by specialized immune system cells. See more: http://COVIDVaccineAnswers.org
Animation created by and for the Vaccine Makers Project. Copyright © 2021, Medical History Pictures, Inc. All rights reserved. The Vaccine Makers Project (VMP) is the classroom-based program of the Vaccine Education Center at the Children’s Hospital of Philadelphia (VEC at CHOP). The Center’s team is composed of scientists, physicians, mothers and fathers devoted to the study and prevention of infectious diseases. The Center was launched in October 2000 to provide accurate, comprehensive and up-to-date information about vaccines and the diseases they prevent. The VMP program is committed to public education about vaccine science via scientifically supported, historically accurate, and emotionally compelling content.
The Vaccine Makers Project gratefully acknowledges the ongoing collaboration and partnership with XVIVO, creator of medical animations and scientific media: https://xvivo.com. Access the VMP’s free classroom materials: http://www.VaccineMakers.org. Find information and resources related to vaccines and their safety: http://vaccine.chop.edu. Learn more about the award-winning documentary for which the original animations were created. The documentary tells the compelling story of one of the world’s most accomplished scientists, Maurice Hilleman: http://www.HillemanFilm.com.
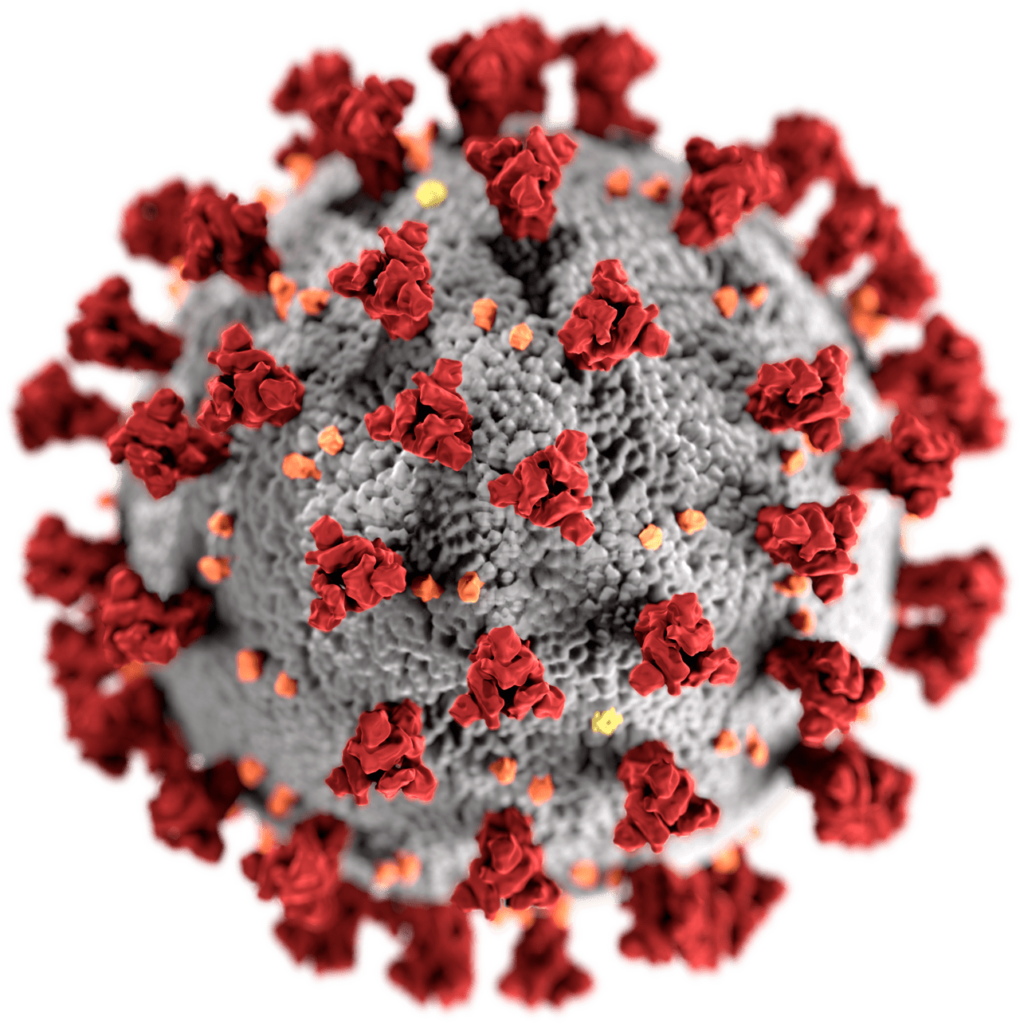
This illustration, created at the Centers for Disease Control and Prevention (CDC), reveals ultrastructural morphology exhibited by coronaviruses. Note the spikes that adorn the outer surface of the virus, which imparts the look of a corona surrounding the virion, when viewed electron microscopically. A novel coronavirus, named Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2), was identified as the cause of an outbreak of respiratory illness first detected in Wuhan, China in 2019. The illness caused by this virus has been named coronavirus disease 2019 (COVID-19). By CDC/ Alissa Eckert, MS; Dan Higgins, MAM #23312.
World Health Organization:
If COVID-19 is spreading in your community, stay safe by taking some simple precautions, such as physical distancing, wearing a mask, keeping rooms well ventilated, avoiding crowds, cleaning your hands, and coughing into a bent elbow or tissue. Check local advice where you live and work. – Do it all!
Make wearing a mask a normal part of being around other people.
Masks should be used as part of a comprehensive strategy of measures to suppress transmission and save lives; the use of a mask alone is not sufficient to provide an adequate level of protection against COVID-19
Here are the basics of how to wear a mask:
- Clean your hands before you put your mask on, as well as before and after you take it off.
- Make sure it covers both your nose, mouth, and chin.
Here are some specifics on what type of mask to wear and when, depending on how much virus is circulating where you live, where you go, and who you are.
- Wear a fabric mask unless you’re in a particular risk group. This is especially important when you can’t stay physically distanced, particularly in crowded and poorly ventilated indoor settings.
- Wear a medical/surgical mask if you:
- Are over 60,
- Have underlying medical conditions
- Are feeling unwell, and/or
- Are looking after an ill family member.
Social distancing
Measures such as social distancing and stay-at-home orders reduce and delay the peak of active cases, allowing more time for healthcare capacity to increase and better cope with patient load.[1] Time gained through thus flattening the curve can be used to raise the line of healthcare capacity to better meet surging demand.[2] By RCraig09 – Own work, CC BY-SA 4.0, Link
Flattening the curve is a public health strategy introduced during the 2019–20 COVID-19 pandemic. The curve being flattened is the epidemic curve, a visual representation of the number of infected people needing health care over time. During an epidemic, a health care system can break down when the number of people infected exceeds the capability of the health care system to take care of them. Flattening the curve means slowing the spread of the epidemic so that the peak number of people requiring care at a time is reduced, and the health care system is not overwhelmed. Flattening the curve relies on mitigation techniques such as social distancing.
In public health, social distancing, also called physical distancing,[2][3][4] is a set of non-pharmaceutical interventions or measures intended to prevent the spread of a contagious disease by maintaining a physical distance between people and reducing the number of times people come into close contact with each other.[2][5] It usually involves keeping a certain distance from others (the distance specified differs from country to country and can change with time) and avoiding gathering together in large groups.[6][7]
By reducing the probability that a given uninfected person will come into physical contact with an infected person, the disease transmission can be suppressed, resulting in fewer deaths.[1][4] The measures are combined with good respiratory hygiene and hand washing.[7][8]

By Toby Morris (Spinoff.co.nz), CC BY-SA 4.0, Link
A complementary measure is to increase health care capacity, to “raise the line”.[3] As described in an article in The Nation, “preventing a health care system from being overwhelmed requires a society to do two things: ‘flatten the curve’—that is, slow the rate of infection so there aren’t too many cases that need hospitalization at one time—and ‘raise the line’—that is, boost the hospital system’s capacity to treat large numbers of patients.”[4] As of April 2020, in the case of the COVID-19 pandemic, two key measures are to increase the number of available ICU beds and ventilators, which are in systemic shortage.[2]
We were all warned about the risk of pandemics
Warnings about the risk of pandemics were repeatedly made throughout the 2000s and the 2010s by major international organizations including the World Health Organization (WHO) and the World Bank, especially after the 2002–2004 SARS outbreak.[5] Governments, including those in the United States and France, both prior to the 2009 swine flu pandemic, and during the decade following the pandemic, both strengthened their health care capacities and then weakened them.[6][7] At the time of the COVID-19 pandemic, health care systems in many countries were functioning near their maximum capacities.[3][better source needed] In a situation like this, when a sizable new epidemic emerges, a portion of infected and symptomatic patients create an increase in the demand for health care that has only been predicted statistically, without the start date of the epidemic nor the infectivity and lethality known in advance.[3] If the demand surpasses the capacity line in the infections per day curve, then the existing health facilities cannot fully handle the patients, resulting in higher death rates than if preparations had been made.[3]
An influential UK study showed that an unmitigated COVID-19 response in the UK could have required up to 46 times the number of available ICU beds.[8] The public health management challenge is to keep the epidemic wave of incoming patients needing material and human health care resources supplied in a sufficient amount that is considered medically justified.[3]
Flattening the curve has Life-saving impact
It is often claimed that “flattening the curve” does not lead to a reduction in the total number of individuals infected during the course of the disease; rather, the infections would only spread over a longer period of time. This is not correct if e. g. the SIR model can be applied to the infection.

SIR model showing the impact of reducing the infection rate (orange) by 76 %By Phrontis – own image, CC BY-SA 3.0, Link
If it’s possible to prevent infections extremely effectively, a significant number of individuals can actually be protected from being infected.
Non-pharmaceutical interventions such as hand washing, social distancing, isolation, and disinfection[3] reduce the daily infections, therefore flattening the epidemic curve. A successfully flattened curve spreads health care needs over time and the peak of hospitalizations under the health care capacity line.[2] Doing so, resources, be it material or human, are not exhausted and lacking. In hospitals, it for medical staff to use the proper protective equipment and procedures, but also to separate contaminated patients and exposed workers from other populations to avoid intra-hospital spread.[3]
Raising the line
Along with the efforts to flatten the curve is the need for a parallel effort to “raise the line” to increase the capacity of the health care system.[2] Health care capacity can be raised by raising equipment, staff, providing telemedicine, home care, and health education to the public.[3] Elective procedures can be canceled to free equipment and staff.[3]
According to Vox, in order to move away from social distancing and return to normal, the US [or any society] needs to flatten the curve by isolation and mass testing and to raise the line.[10] Vox encourages building up health care capability including mass testing, software, and infrastructures to trace and quarantine infected people, and scaling up cares including by resolving shortages in personal protection equipment, face masks.[10]
When to Quarantine
Stay home if you might have been exposed to COVID-19
Quarantine is used to keep someone who might have been exposed to COVID-19 away from others. Quarantine helps prevent the spread of disease that can occur before a person knows they are sick or if they are infected with the virus without feeling symptoms. People in quarantine should stay home, separate themselves from others, monitor their health, and follow directions from their state or local health department.
Quarantine or isolation: What’s the difference?
Quarantine keeps someone who might have been exposed to the virus away from others.
Isolation keeps someone who is infected with the virus away from others, even in their home.
Who needs to quarantine?
People who have been in close contact with someone who has COVID-19—excluding people who have had COVID-19 within the past 3 months.
People who have tested positive for COVID-19 do not need to quarantine or get tested again for up to 3 months as long as they do not develop symptoms again. People who develop symptoms again within 3 months of their first bout of COVID-19 may need to be tested again if there is no other cause identified for their symptoms.
What counts as close contact?
- You were within 6 feet of someone who has COVID-19 for a total of 15 minutes or more
- You provided care at home to someone who is sick with COVID-19
- You had direct physical contact with the person (hugged or kissed them)
- You shared eating or drinking utensils
- They sneezed, coughed, or somehow got respiratory droplets on you
Steps to take: Stay home and monitor your health
- Stay home for 14 days after your last contact with a person who has COVID-19
- Watch for fever (100.4◦F), cough, shortness of breath, or other symptoms of COVID-19
- If possible, stay away from others, especially people who are at higher risk for getting very sick from COVID-19
Cases of reinfection of COVID-19 have been reported but are rare. In general, reinfection means a person was infected (got sick) once, recovered, and then later became infected again. Based on what we know from similar viruses, some reinfections are expected.
References
- Wiles, Siouxsie (2020-03-09). “The three phases of Covid-19—and how we can make it manageable”. The Spinoff. Morningside, Auckland, New Zealand. Archived from the original on 2020-03-27. Retrieved 2020-03-09.
- ^ Jump up to:a b c d Barclay, Eliza (2020-04-07). “Chart: The US doesn’t just need to flatten the curve. It needs to “raise the line.””. Vox. Retrieved 2020-04-07.
- ^ Jump up to:a b c d e f g h i Osmosis.org; Lifebridge Health. Beating Coronavirus: Flattening the Curve, Raising the Line(YouTube video). Retrieved 2020-04-12.
- ^ Jump up to:a b Gelardi, Chris (2020-04-09). “Colonialism Made Puerto Rico Vulnerable to Coronavirus Catastrophe”. ISSN 0027-8378. Retrieved 2020-04-12.
- ^ “Wanted: world leaders to answer the coronavirus pandemic alarm”. South China Morning Post. 31 March 2020. Archived from the original on 9 April 2020. Retrieved 6 April 2020.
- ^ Manjoo, Farhad (25 March 2020). “Opinion | How the World’s Richest Country Ran Out of a 75-Cent Face Mask”. The New York Times. ISSN 0362-4331. Archived from the original on 25 March 2020. Retrieved 25 March 2020.
- ^ “Pénurie de masques : une responsabilité partagée par les gouvernements” [Lack of masks: a responsibility shared by governments]. Public Senat (in French). 23 March 2020. Archived from the original on 2020-04-09. Retrieved 6 April 2020.
- ^ Imperial College COVID-19 Response Team (16 March 2020). “Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand” (PDF). Archived (PDF) from the original on 16 March 2020. Retrieved 23 March 2020.
- ^ Roberts, Siobhan (2020-03-27). “Flattening the Coronavirus Curve”. The New York Times. ISSN 0362-4331. Retrieved 2020-04-12.
- ^ Jump up to:a b Lopez, German (2020-04-10). “Why America is still failing on coronavirus testing”. Vox. Retrieved 2020-04-12.



28 Comments
Pingback: casino online debit card
Pingback: A heavily mutated covid variant in South Africa raises concern - Bergensia
Pingback: sildenafil citrate tablets 50 mg
Pingback: cialis generic cvs
Pingback: cialis 30 x 5 mg us pharmacy
Pingback: best price for viagra 100mg
Pingback: difference between cialis and cialis professional
Pingback: how to buy real cialis online
Pingback: pink viagra tablets
Pingback: 3greener
Pingback: buy ivermectin for scabies
Pingback: ivermectin liquid
Pingback: covid ivermectin
Pingback: tadalafil generic name
Pingback: coupons for ivermectin
Pingback: lucky land casino slot
Pingback: stromectol 12mg online
Pingback: can you buy stromectol over the counter
Pingback: amazon ivermectina para humanos
Pingback: stromectol generic name
Pingback: how much does ivermectin cost
Pingback: price of ivermectin
Pingback: ivermectin dr pierre kory
Pingback: ivermectin new zealand
Pingback: cheap generic cialis from canada
Pingback: dexis ivermectin
Pingback: ivermectin price usa
Pingback: stromectol for scabies