
Ensure healthy lives and promote well-being for all at all ages

Fossil fuels cause 4.5 million premature deaths each year, cost $8 billion every day, cause 40,000 deaths of children younger than 5, and result in 1.8 billion days of work lost from illnesses related to PM2.5.
Greenpeace Southeast Asia. (2020). Toxic air: The price of fossil fuels (full report)
PM2.5 : fine inhalable particles, with diameters that are generally 2.5 micrometers and smaller.
This little story illustrates why the ancient Greeks did not distinguish between science and art:
Updated December 3, 2025, 2024 & 2023 (originally posted December 2, 2021)
Global health progress is slowing after decades of gains. Between 2000 and 2019, maternal and child mortality declined significantly; the HIV incidence rate fell; and healthy life expectancy increased by over five years. However, COVID-19 reversed some of these gains, cutting life expectancy by 1.8 years and slowing progress towards nearly all health-related SDG targets.
Deep inequalities and underresourced systems persist. Despite a growing health workforce and expanded services, major inequalities persist. Low-income and fragile settings face the highest risks due to underfunded systems, service gaps, and workforce shortages. Global health resilience requires bold investment and equity. To meet global health targets by 2030, a substantial intensification of efforts is needed to address deep-seated inequalities, strengthen primary care, build resilient and inclusive health systems, and ensure universal access to quality care.
Under-5 and neonatal mortality rates have improved significantly since 2000, offering the potential to save millions more lives if progress accelerates. HIV-related deaths have halved since 2010, but millions of people still lack treatment, and global positive trends hide data showing that rates of new infections are rising in several regions. Neglected tropical diseases affect nearly 1.5 billion people globally. Achieving universal health coverage requires a greater commitment to reach those furthest behind.
The United Nations is advancing universal health coverage and promoting equitable, people-centred health systems, focusing on fragile, conflict-affected regions and areas with significant health inequalities. Through initiatives such as the Joint United Nations Programme on HIV/AIDS (UNAIDS) and the World Health Organization roadmap for neglected tropical diseases 2021–2030, the United Nations targets the most underserved populations. It has also led efforts in pandemic preparedness and is intensifying action on mental health as a core component of overall well-being.
Target 3.1 – The global maternal mortality ratio decreased from 228 maternal deaths per 100,000 live births in 2015 to 197 in 2023. To reach the global target of 70 per 100,000 live births, nearly 700,000 deaths need to be prevented between 2024 and 2030. The proportion of births attended by skilled health personnel has increased from 80 per cent in 2015 to 87 per cent in 2024.
Target 3.2 – In 2023, the number of global under-5 deaths was 4.8 million, down from 10.1 million in 2000 and 6.2 million in 2015. The under-5 mortality rate dropped to 37 deaths per 1,000 live births, which represents a decline of 52 per cent since 2000 and 16 per cent since 2015. Similarly, the neonatal mortality rate fell to 17 deaths per 1,000 live births in 2023 – a decrease of 44 per cent since 2000 and 12 per cent since 2015. Meeting targets in relation to the Goals could save 8 million lives by 2030.
Target 3.3 – In 2023, 39.9 million people were living with HIV, but 9.3 million lacked life-saving treatment. As a result, one person dies from AIDS-related causes every minute. AIDS-related deaths halved between 2010 and 2023, from 1.3 million to 630,000. During this period, new HIV infections dropped by 39 per cent globally. It should be noted, however, that infections are rising in the Middle East and North Africa, Eastern Europe, Central Asia, and Latin America.
Globally, 8.2 million people were reported as newly diagnosed with tuberculosis in 2023. This was the highest number for a single year since data became available in the mid-1990s, up from the previous record of 7.5 million in 2022, and 15 per cent higher than in 2019.
Since 2000, an estimated 2.2 billion malaria cases and 12.7 million deaths have been averted worldwide. By the end of 2024, 44 countries and one territory had been certified as malaria-free.
In 2023, 1.495 billion people required interventions against neglected tropical diseases, including 493 million in the least developed countries, which was 122 million fewer than in 2022. By December 2024, 54 countries and territories had eliminated at least one neglected tropical disease.
Target 3.4 – Globally, in 2021, it is estimated that 18 million people under the age of 70 died from a noncommunicable disease. This figure represents more than half of the deaths among people in this age range. The risk of premature death from any of the four primary noncommunicable diseases (cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes) has decreased since 2015, but, despite increased awareness, the world is not on track to meet the target for the reduction of noncommunicable diseases by 2030.
Target 3.7 – The global adolescent birth rate among girls between the ages of 15 and 19 fell from 66.3 per 1,000 in 2000 to 38.3 per 1,000 in 2024, and is projected to decline to 34.8 by 2030. Among girls aged 10-14, the rate dropped from 3.5 to 1.0 per 1,000 over the period 2000–2024. Despite this progress, the highest rates were reported in sub-Saharan Africa, at 92.9 per 1,000 for the 15–19 age range. and 3.1 per 1,000 for the 10–14 age range.
Target 3.b – Progress stagnated or dipped between 2020 and 2022 with respect to all four childhood vaccines covered by indicator 3.b.1. For the third dose of the vaccine containing diphtheria, tetanus and pertussis, which is a useful marker of how well a vaccination system is functioning, performance had still not been fully restored, by 2023, to the pre-pandemic level seen in 2019. Coverage rates for the other three vaccines increased, but this was partly due to vaccines being introduced in countries where they were previously unavailable. The global target of 90 per cent set by the Immunization Agenda 2030 is unlikely to be met for any of these vaccinations if current trends continue.

Target 3.c – The global health workforce surpassed 70 million in 2023, with 52 million people working in key professions, such as dentists, medical doctors, midwives, nurses, and pharmacists. Density in the key professions has increased by 26 per cent since 2013. Health worker density ranges from 1 per 64 people in high-income countries to 1 per 621 in low-income ones. Globally, a shortage of 11.1 million health workers is projected in 2030, with countries in Northern Africa and sub-Saharan Africa accounting for over half of the shortage.

A toxic haze has smothered Delhi since the festival of Diwali.
BBC: Authorities in the Indian capital, Delhi, have closed all schools and colleges indefinitely due to worsening air pollution.
Construction work was banned until 21 November, but an exception was made for transport and defense-related projects. Only five of the 11 coal-based power plants in the city have been allowed to operate.
The levels of PM2.5 – tiny particles that can clog people’s lungs – in Delhi are far higher than the World Health Organization’s (WHO) safety guidelines. Several parts of the city recorded figures close to or higher than 400 on Tuesday, categorized as “severe.”
Some schools had already closed last week because of pollution, and the Delhi government said it was considering a lockdown to improve air quality as dense clouds of smog engulfed the city.
A mix of factors, such as vehicular and industrial emissions, dust, and weather patterns, make Delhi the world’s most polluted capital. The air turns especially toxic in the winter months as farmers in neighboring states burn crop stubble. Fireworks during the Diwali festival, which happens at the same time, only worsen the air quality. Low wind speed also plays a part in trapping pollutants in the lower atmosphere.
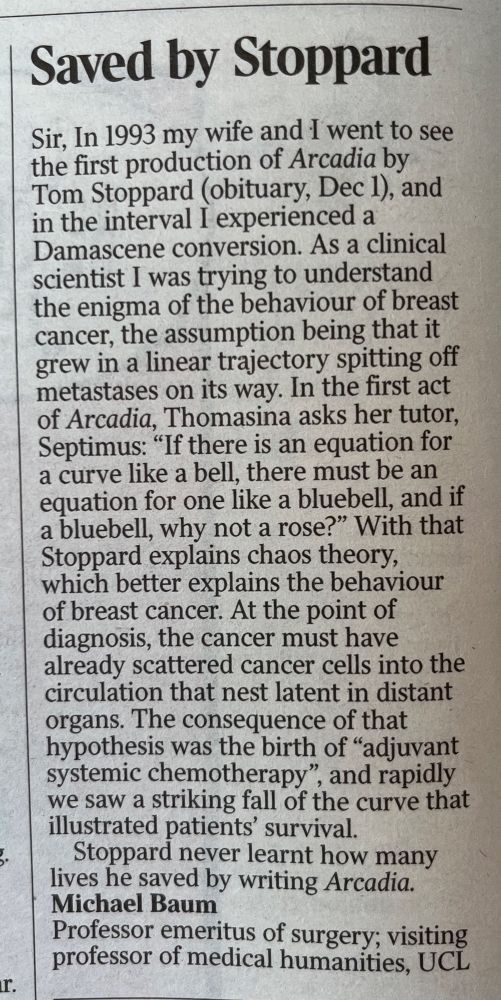
How is air quality measured?
Air quality is determined by the levels of air pollutants PM2.5, PM10, ozone, nitrogen dioxide, sulfur dioxide, and carbon monoxide.
Particulate matter (PM) comprises tiny particles that negatively impact health. PMs vary in size, the most damaging are PM2.5 and PM10 – with a diameter of less than 2.5 μm and 10μm respectively. A human hair’s diameter is 50-70 μm. PM2.5 levels lower than 12 are considered good, 55-150 unhealthy and 250 or above is hazardous.
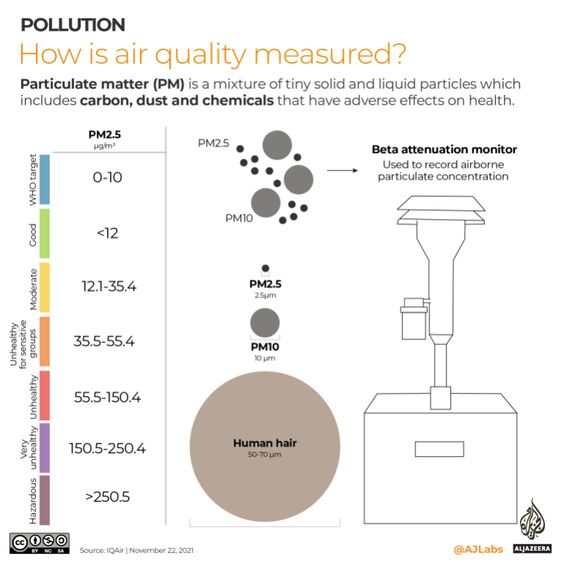
India’s deadly pollution
According to the Lancet, in 2019, 1.67 million deaths in India were caused by air pollution.
While replacing solid fuels with alternatives has lowered deaths linked to household air pollution since 1990, deaths related to ambient PMs have increased.
Fifteen of the 20 most polluted cities are in India, mainly in the north. Stubble burning spikes pollution in autumn and winter. Vehicle emissions, industry, and burning rubbish also contribute to high levels of PM2.5 and other pollutants.
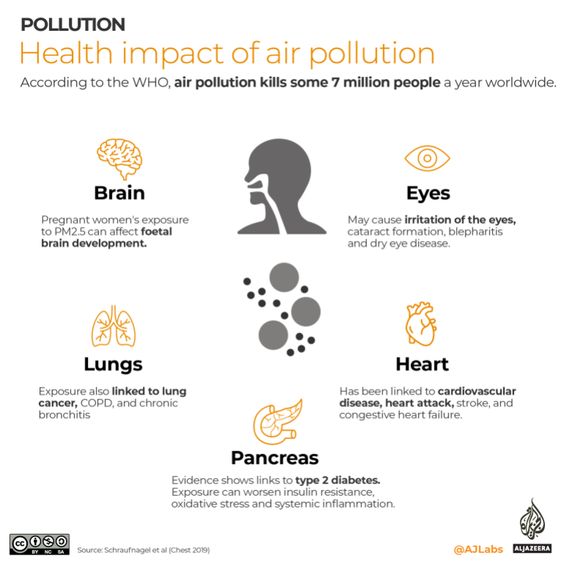
Air pollution’s health impacts
According to the WHO, some 7 million people die annually from air pollution. More than 90 percent of the world’s population lives in areas where air pollution exceeds WHO limits. Air pollution is linked to several illnesses, including asthma, diabetes, and heart disease.
United Nations Global Goals for Sustainable Development
Great strides have been made in improving people’s health in recent years. 146 out of 200 countries or areas have already met or are on track to meet the SDG target on under-5 mortality. Effective HIV treatment has cut global AIDS-related deaths by 52 percent since 2010, and at least one neglected tropical disease has been eliminated in 47 countries.
However, inequalities in healthcare access persist. The COVID-19 pandemic and other ongoing crises have impeded progress towards Goal 3. Childhood vaccinations have experienced the most significant decline in three decades, and tuberculosis and malaria deaths have increased compared with pre-pandemic levels.
The Sustainable Development Goals boldly commit to ending the epidemics of AIDS, tuberculosis, malaria, and other communicable diseases by 2030. The aim is to achieve universal health coverage and provide access to safe and affordable medicines and vaccines for all.
Increased investment in health systems is needed to overcome these setbacks and address long-standing healthcare shortcomings, support countries in their recovery, and build resilience against future health threats.
Access to essential health services
A significant portion of the global population still lacks access to vital healthcare services. Addressing disparities is critical to bridging this gap and ensuring equitable healthcare provision. Various determinants of health, including environmental and commercial factors, need attention to achieve our common objective of Health for all and the Sustainable Development Goal targets.
Before the pandemic, major progress was made in improving the health of millions of people. Significant strides were made in increasing life expectancy and reducing some of the common killers associated with child and maternal mortality. However, more efforts are needed to eradicate a wide range of diseases and address many different persistent and emerging health issues. By focusing on providing more efficient funding for health systems, improved sanitation and hygiene, and increased access to physicians, significant progress can be made in helping save millions of lives.
Health emergencies such as COVID-19 pose a global risk and have shown the critical need for preparedness. The United Nations Development Programme highlighted huge disparities in countries’ abilities to cope with and recover from the COVID-19 crisis. The pandemic provides a watershed moment for health emergency preparedness and investment in critical 21st-century public services.
COVID-19 response
The World Health Organization (WHO) has led the global effort to tackle COVID-19. The Strategic Preparedness and Response Plan, produced by WHO and partners, outlines the public health measures countries should take to prepare for and respond to COVID-19. The Strategy Update of April 2020 provides further guidance for the public health response to COVID-19 at national and sub-national levels. It highlights the coordinated support required from the international community to meet the challenge of COVID-19.
People and organizations who want to help fight the pandemic and support WHO and partners can donate through the COVID-19 Solidarity Response Fund. This fund supports WHO’s work to track and understand the spread of the virus, ensure patients get the care they need, ensure frontline workers get essential supplies and information, and accelerate research and development of a vaccine and treatments for all who need them.
WHO, together with partners, also provides guidance and advice for people to look after their mental health during the COVID-19 pandemic — especially health workers, managers of health facilities, people looking after children, older adults, people in isolation, and members of the public more generally.
The pandemic is much more than a health crisis. It requires a whole-of-government and whole-of-society response, matching the resolve and sacrifice of frontline health workers.
Facts and Figures
Child health
- In 2018, an estimated 6.2 million children and adolescents under the age of 15 years died, mostly from preventable causes. Of these deaths, 5.3 million occurred in the first 5 years, with almost half of these in the first month of life.
- Despite determined global progress, an increasing proportion of child deaths are in Sub-Saharan Africa and Southern Asia. Four out of every five deaths of children under age five occur in these regions.
- Children in sub-Saharan Africa are more than 15 times more likely to die before the age of 5 than children in high-income countries.
- Malnourished children, particularly those with severe acute malnutrition, have a higher risk of death from common childhood illnesses such as diarrhea, pneumonia, and malaria. Nutrition-related factors contribute to about 45 percent of deaths in children under 5 years of age.
Maternal health
- Over 40 percent of countries have fewer than 10 medical doctors per 10,000 people, and over 55 percent have fewer than 40 nursing and midwifery personnel per 10,000 people.
- In Eastern Asia, Northern Africa, and Southern Asia, maternal mortality has declined by around two-thirds.
- Every day in 2017, approximately 810 women died from preventable causes related to pregnancy and childbirth.
- 94 percent of all maternal deaths occur in low and lower-middle-income countries.
- Young adolescents (ages 10-14) face a higher risk of complications and death as a result of pregnancy than other women.
- But the maternal mortality ratio – the proportion of mothers who do not survive childbirth compared to those who do – in developing regions is still 14 times higher than in the developed regions.
HIV/AIDS, malaria, and other diseases
- 38 million people globally were living with HIV in 2019.
- 25.4 million people were accessing antiretroviral therapy in 2019.
- 1.7 million people became newly infected with HIV in 2019.
- 690 000 people died from AIDS-related illnesses in 2019.
- 75.7 million people have become infected with HIV since the start of the epidemic.
- 32.7 million people have died from AIDS-related illnesses since the start of the epidemic.
- Tuberculosis remains the leading cause of death among people living with HIV, accounting for around one in three AIDS-related deaths.
- Globally, adolescent girls and young women face gender-based inequalities, exclusion, discrimination and violence, which put them at increased risk of acquiring HIV.
- HIV is the leading cause of death for women of reproductive age worldwide.
- AIDS is now the leading cause of death among adolescents (aged 10–19) in Africa and the second most common cause of death among adolescents globally.
- Over 6.2 million malaria deaths have been averted between 2000 and 2015, primarily of children under five years of age in sub-Saharan Africa. The global malaria incidence rate has fallen by an estimated 37 percent and the mortality rates by 58 percent.
Goal 3 Targets
3.1 By 2030, reduce the global maternal mortality ratio to less than 70 per 100,000 live births.
3.2 By 2030, end preventable deaths of newborns and children under 5 years of age, with all countries aiming to reduce neonatal mortality to at least as low as 12 per 1,000 live births and under-5 mortality to at least as low as 25 per 1,000 live births.
3.3 By 2030, end the epidemics of AIDS, tuberculosis, malaria, and neglected tropical diseases and combat hepatitis, water-borne diseases, and other communicable diseases.
3.4 By 2030, reduce by one-third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being.
3.5 Strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol.
3.6 By 2020, halve the number of global deaths and injuries from road traffic accidents.
3.7 By 2030, ensure universal access to sexual and reproductive healthcare services, including family planning, information and education, and the integration of reproductive health into national strategies and programs.
3.8 Achieve universal health coverage, including financial risk protection, access to quality essential healthcare services, and access to safe, effective, quality, and affordable essential medicines and vaccines for all.
3.9 By 2030, substantially reduce the number of deaths and illnesses from hazardous chemicals and air, water, and soil pollution and contamination.
3.A Strengthen the implementation of the World Health Organization Framework Convention on Tobacco Control in all countries, as appropriate.
3.B Support the research and development of vaccines and medicines for the communicable and non-communicable diseases that primarily affect developing countries, provide access to affordable essential medicines and vaccines, in accordance with the Doha Declaration on the TRIPS Agreement and Public Health, which affirms the right of developing countries to use to the full the provisions in the Agreement on Trade Related Aspects of Intellectual Property Rights regarding flexibilities to protect public health, and, in particular, provide access to medicines for all.
3.C Substantially increase health financing and the recruitment, development, training, and retention of the health workforce in developing countries, especially in the least developed countries and small island developing States.
3.D Strengthen the capacity of all countries, in particular developing countries, for early warning, risk reduction, and management of national and global health risks.
Links
WHO – Reducing Child Mortality
UNFPA Sexual & reproductive health





1 Comment
Pingback: winter morning jazz